Ambulance
Gesundheit + Medizin, Dokumentation •
14.11.2024 • 22:00 - 23:00 heute
Originaltitel
Ambulance
Produktionsland
GB
Produktionsdatum
2024
Gesundheit + Medizin, Dokumentation
The shift begins with Homerton-based crew Niamh and Isobel and clinical team manager Gary being dispatched to a 25-year-old patient who has fallen from height whilst scaling the walls at a climbing centre. He needs urgent treatment to put broken bones back in alignment, otherwise he might lose a limb. Rob and Nikita are another of the 70 frontline crews also working through the night to provide care to people in north east London. As the dispatch team deal with a surge in calls leading to ever-lengthening response times, Rob and Nikita are sent to care for a 77-year-old patient who has been stuck on the floor for five hours. The crew discover he is suffering from an irregular heart beat and requires further treatment at hospital. Despite their efforts to persuade him, the patient is not convinced he should be in hospital, and they reluctantly agree to leave him at home. With none of their critical care resources available, the London Ambulance Service call upon the HEMS team to aid Niamh and Isobel as they provide life support to a 62-year-old male who is having a seizure following a fall. As the specialist pre-hospital doctors try to save the patient's life at the roadside, Niamh and Isobel balance the patient's medical needs with providing comfort and support to his partner, who is watching on as events unfold. As crews continue to work through the backlog of emergencies, Rob and Nikita are dispatched to a 37-year-old female with Rett syndrome, a rare genetic disorder that impedes brain development. The crew are touched to hear the positive impact the ambulance service has had on the patient's life as they discover the severity of unrelenting challenges that come with the life-limiting disability. The ambulance service is grappling with sustained high demand - answering a new 999 call every four seconds - when a 30-person fight breaks out in Woodford Green. As the fight further depletes the resources available, crewmates Faheema and Steve and clinical team manager Gary are dispatched to a serious RTC involving a HGV and taxi. En route, Gary shares his trepidation heading into big incidents as he recalls being one of the first on the scene during the 2017 London Bridge terror attacks: "The number of patients outweighed what I could offer. You need to prioritise and triage the patients, and that ultimately means walking past patients who are dying but beyond help at that point." Mental health is prevalent in the early hours of the morning, and Rob and Nikita are dispatched to a patient in crisis. With his anxiety levels at an all-time high, the patient's family have run out of options, and they believe their only hope lies with the ambulance service. Rob takes the time to listen to the patient, giving them time to share their story and going above and beyond to ensure they have an effective care plan in place. During the job, Rob reflects on the importance of communication when caring for patients: 'We're all different... it's about trying to find any avenue to actually connect with that patient, to be like, you can trust me, let's go.' This episode explores how the modern-day ambulance service contributes hugely towards community care, while also showcasing advances in pre-hospital emergency medicine, which allow senior clinicians to perform pioneering interventions at the roadside. We see frontline workers adapting their care practice to suit each patient they meet, ensuring that everyone feels listened to, respected, and treated with skill and compassion.
Film-Archiv

Twisters
Actionthriller • 2024
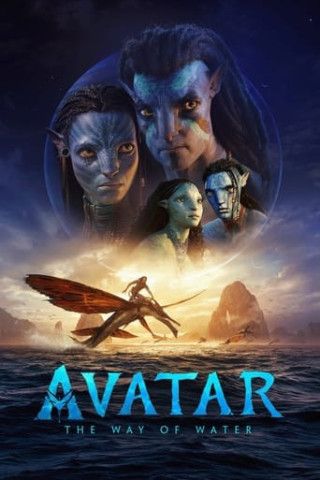
Avatar: The Way of Water
Science-Fiction • 2022
Alles steht Kopf
Spielfilm • 2015

Das Erwachen der Jägerin
Drama • 2023

Deadpool & Wolverine
Sciencefiction-Komödie • 2024

Wonka
Komödie • 2023
Arthur der Große
Drama • 2024
The Creator
Scifi-Action • 2023
Findet Nemo
Trickfilm • 2003
2 Guns
Actionthriller • 2013
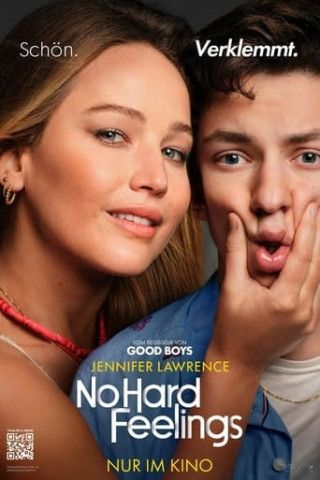
No Hard Feelings
Komödie • 2023

Eine Million Minuten
Drama • 2024
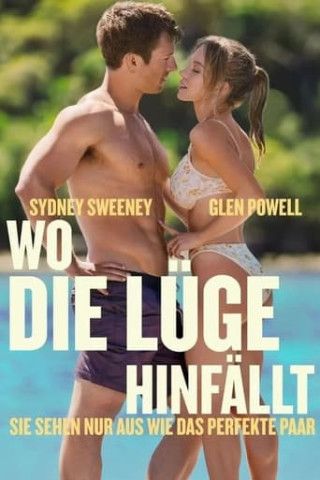
Wo die Lüge hinfällt
Komödie • 2023
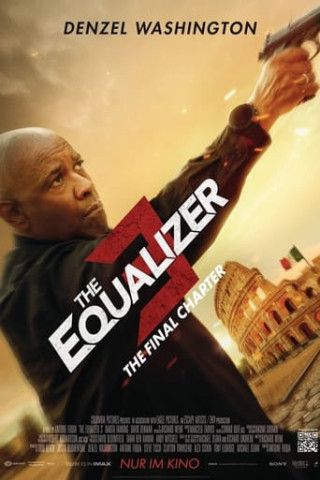
The Equalizer 3
Actionfilm • 2023

Argylle
Komödie • 2024